Let’s cut to the chase; modern life or more accurately, physical inactivity, is killing us?
Well yes, the World Health Organization (WHO) has made a statement that physical inactivity is now the major cause of non-communicable diseases in the world, and we have to do something about it. One of the biggest challenges we have in our society is being able to sustain our healthcare system with an ageing population and a population that, with the industrial age and now the technological age, has become less and less physically active. The only chance we have of reversing this trend towards not being able to cover the costs of healthcare is by addressing some of the underlying causes of our current problems.
Such as physical inactivity – what health problems are we talking about?
Cardiovascular disease, metabolic syndrome, obesity, type 2 diabetes, some cancers. There is now sufficient research to show that physical inactivity can lead to these conditions, but also that the onset of them can be managed and even reversed with physical exercise. And also, even after people have been diagnosed and they’ve, for example, started taking diabetic medication or had surgery and chemotherapy for cancer, exercise can help them manage their condition and/or recover from it.
The recuperative power of exercise – how strong is the evidence?
For cancer, studies are showing that physical exercise, performed before or after the diagnosis, is related to an astonishing reduction in mortality risk of 40-50 per cent for breast and colorectal cancer survivors. Research is also now suggesting similar effects for prostate cancer. Aerobic exercise for stroke patients has been shown to improve their mobility, but also their cardiovascular fitness. Which is significant, as it used to be thought that the latter couldn’t be achieved because of the disability caused by the stroke. But stroke is often the result of cardiovascular disease, and improving fitness can address some of the risk factors associated with having another stroke. Exercise has also been shown to improve the mobility of people with osteoarthritis, and reduce pain. The list goes on.
You’ve described exercise as a form of medicine?
Medicine has always been based on the idea that if you have a problem, you go see a doctor, and the doctor will give you something to take or do, and that’s that. One of the major mindsets that society has to overcome, when it comes to conditions caused by physical inactivity, is that the traditional health model doesn’t work anymore.
Haven’t we always known that exercise is good for us?
True, although when we first recognized this is hard to say; some have referred to Plato. But we’re now starting to better understand the science, such as the cognitive benefits of exercise, and how exercise can balance some of the inflammation processes that go on in our body, which helps us manage pain and autoimmune diseases. We’re starting to understand how exercise is affecting some of the metabolic components like cholesterol, high blood pressure and so on. But we’ve not yet arrived at the point when the community as a whole realize how serious a problem physical inactivity can be.
So we need to change the model of healthcare?
Yes, and it has begun to change. “Green” prescription is an attempt to do this. If you go to your doctor and you’re overweight, and your cholesterol is borderline and you’re setting yourself up for cardiovascular disease, your doctor might give you a referral to a gym or another organization, where you can join an exercise group and become more active. The problem is that the people who need exercise the most are not going to get the level of attention and specialized professional exercise help they might need.
Which is where clinical exercise physiologists come in. But what do they do exactly?
It’s about prescribing exercise to help people manage a range of health conditions, but it’s very individualized. For example, we might take a person and assess their cardiorespiratory fitness, their other abilities and disabilities, and prescribe a program of safe exercise designed to lift that person’s cardiorespiratory fitness to a level that is appropriate for someone at their age. That’s a very specialized job. A doctor might tell you to go to your local gym, but if you have a medical condition that really needs a specific and individualized exercise prescription, you should go to an expert, a clinical exercise physiologist.
But we have national guidelines on what we need to do, say, walk for half an hour five times/week, perhaps add in a couple of swims. What does a clinical exercise physiologist offer above that?
The people that do that level of exercise are probably well on their way to doing the best they can for themselves, but the problem is that they’re following some kind of standard guideline. It doesn’t tell you anything about yourself. I could walk for 150 minutes a week, but it might have little positive effect on my cholesterol or type 2 diabetes, because I might need twice that amount of exercise. If you want to get the optimal benefit from exercise, it has to be prescribed for you and your condition, and it needs to be monitored. That’s where the skill of the clinical exercise physiologist comes in; it’s about taking the individual, and making sure the dose and type of exercise is optimal.
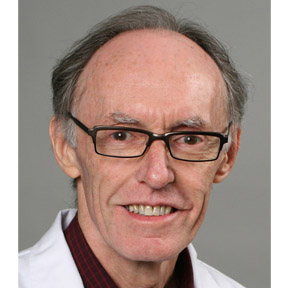
Jim Stinear is Associate Professor at Auckland University’s Department of Exercise Sciences, and academic director of the Master’s degree program in Clinical Exercise Physiology, which is focused on the therapeutic use of exercise in the prevention, management and rehabilitation of chronic conditions, diseases, injuries and chronic pain.
If you want more health and fitness inspiration simply sign up to Fit Planet and get the freshest insights and advice straight to your inbox.